Published Date:
Mar 24, 2023
Exclusive
Value-Based Care
AI
Behavioral Health
Why value-based care is the most misunderstood concept in healthcare.
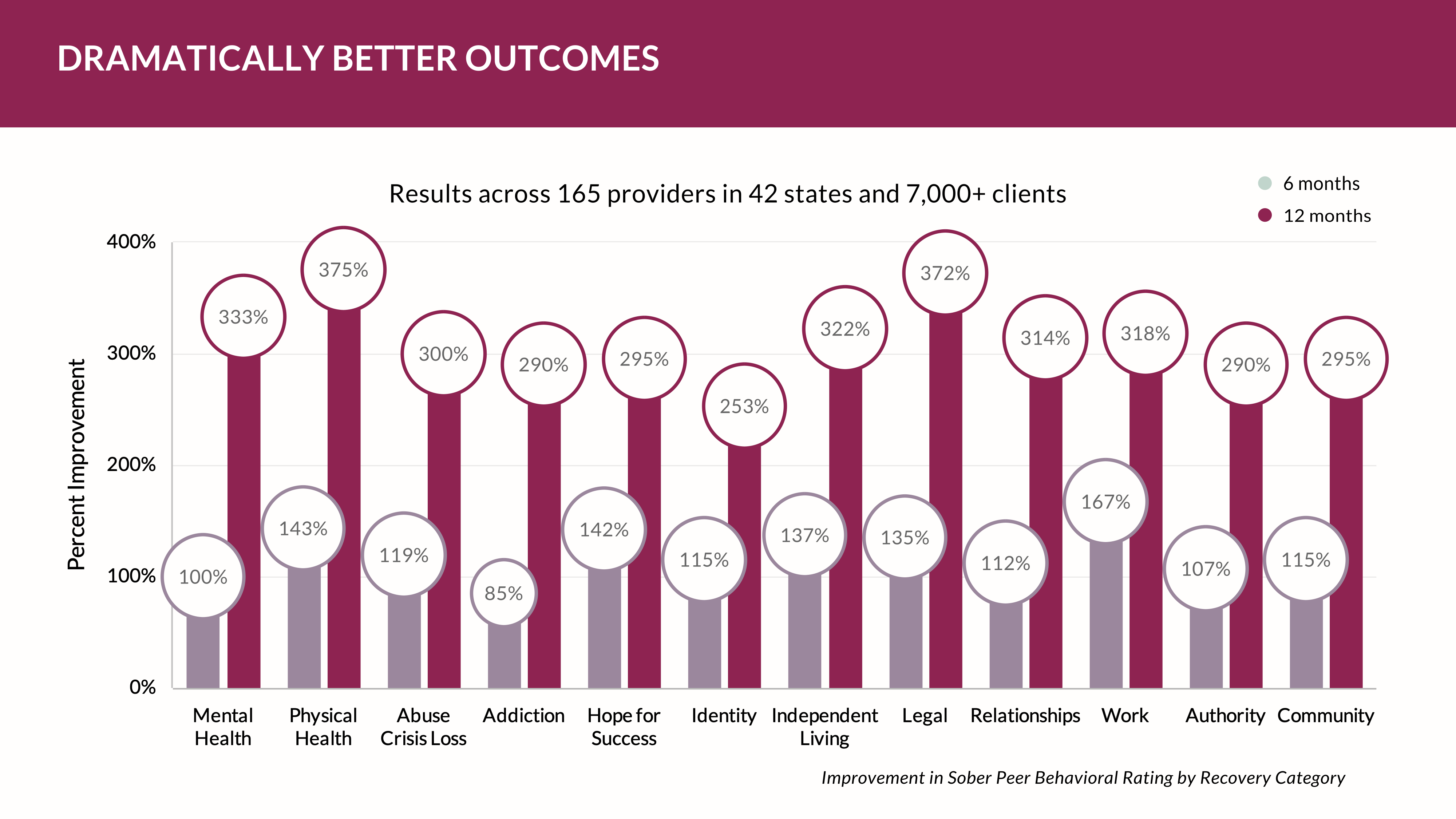
Value-based care, which prioritizes patient outcomes over the quantity of services provided, is often misunderstood due to its complex and multifaceted nature, as well as the significant changes it requires in healthcare delivery and payment systems. This has led to challenges in implementing and scaling value-based care initiatives across the healthcare industry.
The healthcare industry is shifting to value-based care. It’s not an “if”. It’s when. Healthcare costs are rising faster than the consumer’s ability to pay the premium for the services of health. So, the insurance industry created something new for providers to worry about. The core concept around value-based care (code for payments) relies on mastering one simple idea: risk. Providers are just beginning to understand how to get their heads around the concept and how to win using it – or more accurately stated, how to avoid it.
But what is risk exactly?
Risk. It sounds so threatening doesn’t it. Insurance companies are masters of risk. Their entire focus is building models to out-smart risk then scaling so large that any risk they own is conveniently spread around. It’s an interesting amalgamation of analytics and instruments (called policies and pools) that are -- in a weird way -- fascinating. Our team once built an insurance product and used in on Wall Street and in doing so got into the mindset of why insurance companies make so much money by avoiding, yes here’s that word again, risk.
But, for healthcare providers it’s not a naturally engrained idea. Providers care for people and want them to get better. So, when the topics of quality of care and risk are put in the same conversation the immediate retort is, “we need better outcomes”. That usually leads to, “we need to measure them”. Then you’ll hear, “this is the best tool – it’s the “evidence based” one! And, finally in shear desperation providers declare, “payers don’t understand our mission”!
Though, despite the variable truth of this, managing risk for getting the highest fee for the quality of service we provide has a lot of moving parts. Those parts aren’t part of the process or systems we commonly use today. Don’t bet on your electronic healthcare record system to manage risk – it wasn’t built for that.
If it’s now our job to avoid risk to get paid for what we do, then how?
The transformative success for providers hinges on building key wrap-around processes that are built for the task at hand. Insurers know this very well. Afterall, they’re in the business of risk. Don’t kid yourself. The partnership between a provider and payer isn’t a fair fight. Nor is it a partnership. It’s about who can prove - in advance - an outcome is virtually assured. Consider these hard realities:
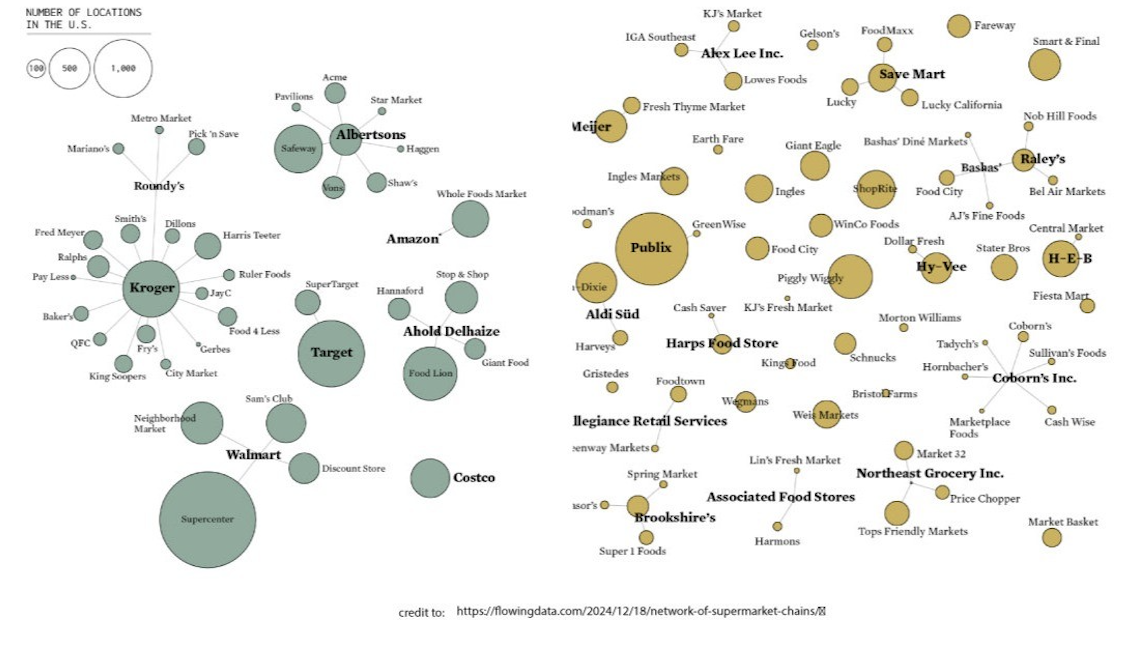
Here’s your first hard reality: most providers are small and do not have scale to win in a risk-based system. Insurers do. Averting risk requires an interconnected scale large enough to prove all the factors that will contribute to catastrophic risk. For that, you’ll need access to large interconnected data formatted in special ways to compete. You’ll have to subscribe to those.
Here’s your second hard reality: most providers aren’t equipped to recognize risk so they can avoid it. Insurers are. They see millions of transactions and that gives them insight on how to move risk around. There’s an Achilles Heal favoring providers here; claim data is so large it’s almost impossible to manage the coming wave of Web3 healthcare – supporting smart contracts that automatically trigger payments based on observable, real time results. Smart Contracts are the future on this new infrastructure. Health Clouds makes small providers nimble so providers can scale using new views of data and smart contracts to make payments fluid and guaranteed.
Here’s your third hard reality: you need to get really good at interoperable IT and data analytics and you’ll need a new infrastructure for that. The aggregation of data from disparate source systems (including clinical, operational, financial, and administrative) will improve transparency across all points of care. Investment here is a must because your payoff will be measured in multiples.
Here are five ways to win at the risk game by using a Health Cloud:
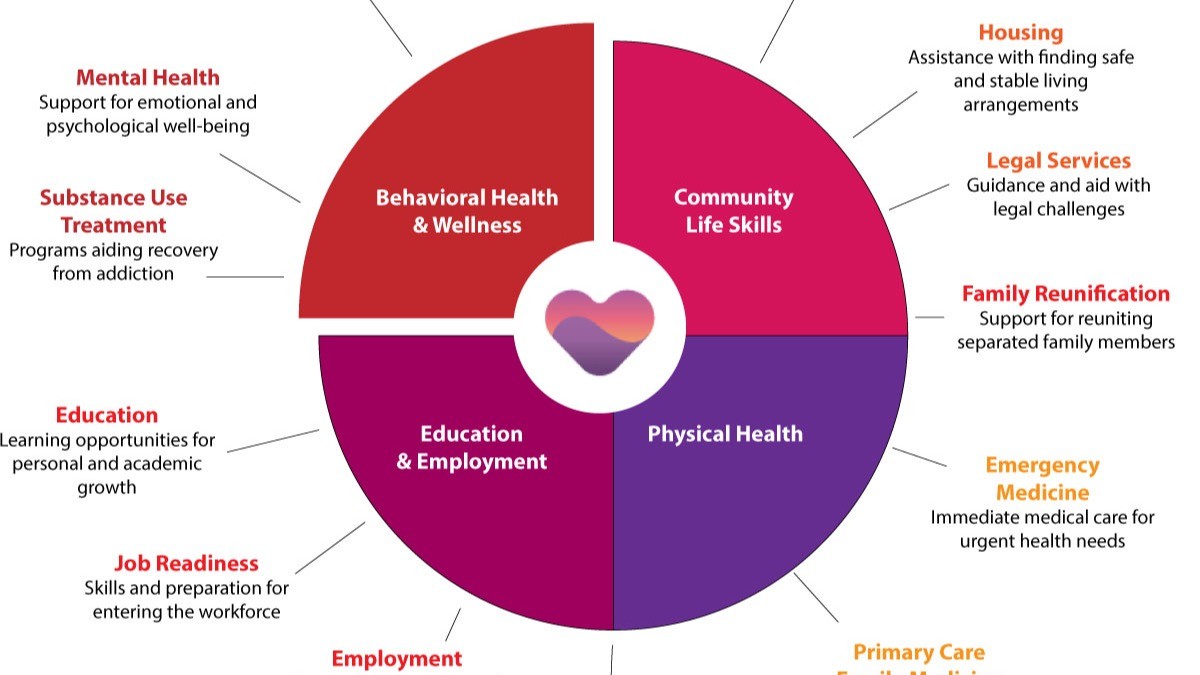
- Value-Based Care Model: As patients become more informed about their own care options, they expect greater value from their healthcare provider or insurer than ever before – which means that providing quality services at an affordable price has never been more important. Transitioning away from traditional fee-for-service models towards a value-based approach where reimbursement is tied directly to successful outcomes will require significant investment into data collection infrastructure as well as analytics capabilities so that performance metrics can be effectively monitored over time. You’re going to need to wrap your Electronic Healthcare Record systems with other tools to compete.
- Patient Engagement Strategies: In addition to providing better care at lower costs, healthcare organizations must also focus on engaging patients. You’ll need scale. The lowest hanging fruit for engagement is digital health. Specifically designing communities around your practice to maximize your risk by distributing it – just like the insurance carriers do. You’ll need an entire Digital Health platform for that. It’s going to be about community care quality going forward.
- Cost Optimization Plans: Cost optimization plans designed to reduce make the best use of expenses without compromising quality patient care is the tool is your next investment because it doesn’t exist in today’s electronic health record systems. You’re going get very familiar with cost accounting so learn to love it.
- Data Security Practices: With vast amounts increasing digitization across industry data security practices to ensure personal confidential information is secure is moving to blockchain and Web3 concepts. Learn about them - quickly.
- Strategic Partnerships & Alliances: Finally strategic partnerships and alliances formed between various stakeholders within sector create communities. Communities will become proprietary and are a hedge to spread risk but to build great practices that are profitable and meaningful. Patients benefit when you build communities for comprehensive coverage and improve access higher levels service.
By mastering each these five core business model changes health providers position themselves to succeed in the challenging environment ahead. In the next five years providers will think like insurers and manage risk similarly.
Other Blogs
The Plan No One Sees Coming—But Soon Will
Exclusive
Mental Health
Addiction
Drugs

Ant Pheromone Study May Improve Mental Health Outcomes
Exclusive
Mental Health
Addiction
Drugs
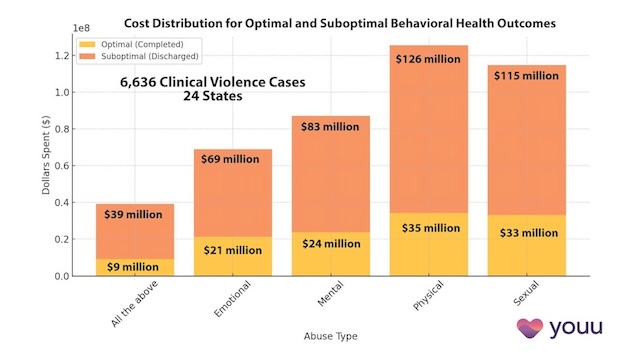
Interrupting Violence Should Be Irresistibly Investable
Exclusive
Mental Health
Addiction
Drugs
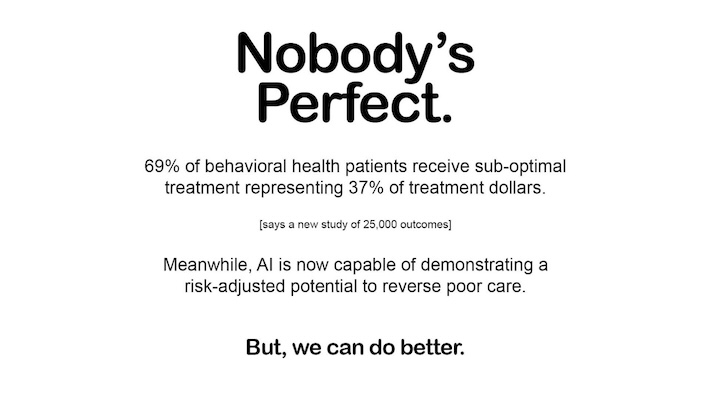
69% of Behavioral Health Patients Receive Sub-Optimal Care According to a New Analysis
Exclusive
Mental Health
Addiction
Drugs
Other Blogs
Have Questions? Lets Meet
Select a time you like to meet with us