Published Date:
Dec 10, 2024
Exclusive
Mental Health
Addiction
Drugs
We Need a Small World for a New World of Healthcare
Navigating healthcare has a purposeful engineering design; control its access and payment options to the point of scarcity to control those in need (code for “fee-for-service”). Those who find themselves stuck navigating a system that feels designed to frustrate, go without. That’s because it is intentional.
Correcting it could be simpler than we think.
Picture the problem like an all-you-can-eat shrimp buffet in Las Vegas, but with only one narrow entrance and a seemingly endless line of eager diners. This is the state of today's healthcare.
The bottleneck isn’t just frustrating—it’s deliberate, controlling the flow of supply (of shrimp) by restricting access (a single doorway) to meet the overwhelming demand (of the hungry). The all-you-can eatery was made famous by casinos. Casinos cleverly figured out how subsidize shrimp by picking your pocket while you wait in line (like the hospital emergency departments acting as backstops for lack of primary care access).
Let’s face it. It’s not surprising that our healthcare is underperforming. Here’s how we can improve it by reengineering the way we approach the problem.
For those of us who find a weird fascination with analytics, there’s a maxim known as the Small World Theory.
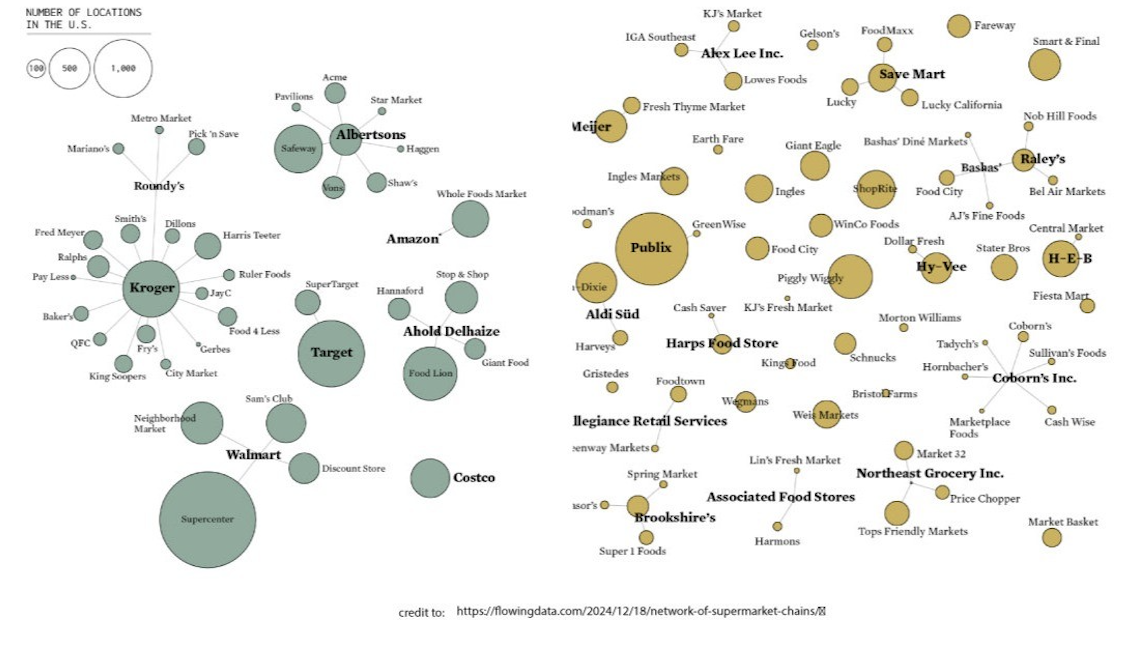
You may recognize by the “six degrees of separation” axiom made popular by the movie with the same name. It posits that everyone in the world is connected through a small number of intermediaries, through a small number of accessible “degrees of separation.” It’s all around us; like LinkedIn or Amazon, or other hybrid many-to-many platform networks like FinTech.
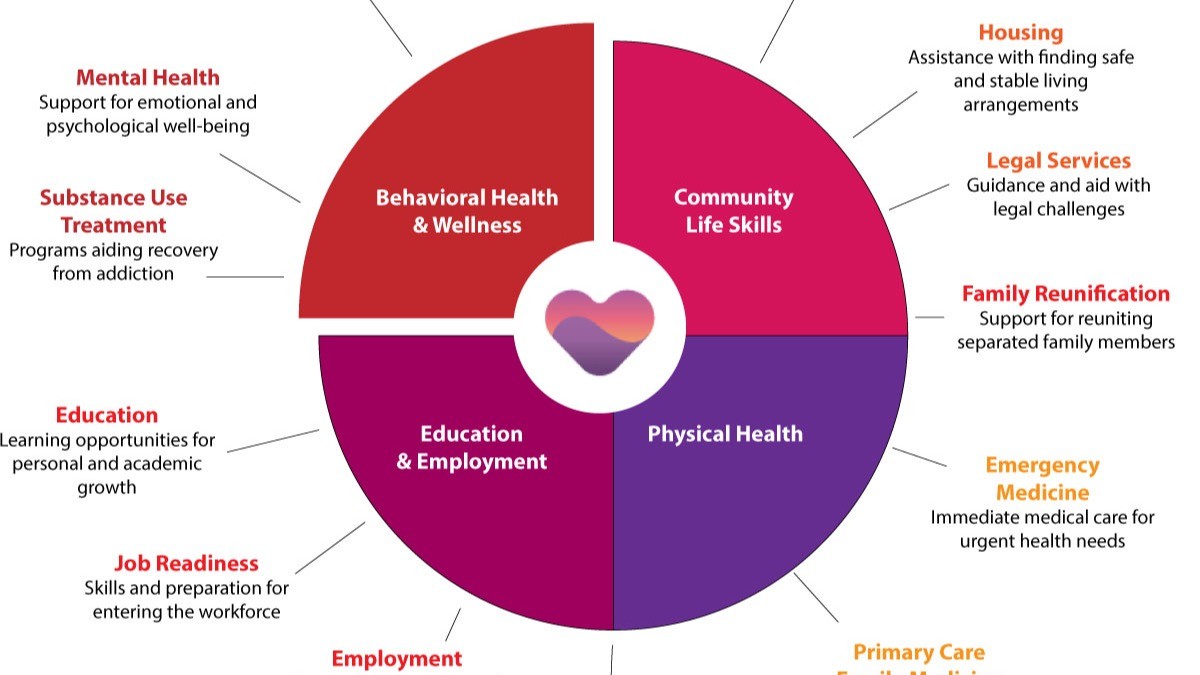
In a healthcare context, this means that even in large, complex systems, people—whether patients, doctors, researchers, or community health workers—are closer to one another than they might seem (like having many doorways at the shrimp buffet).
For example, a patient in a remote rural area could, through just a few connections, be linked to a leading specialist in a distant city or an innovative public health program in their community. This interconnectedness (measured in degrees of separation) provides a unique opportunity to improve population health through collaboration and information sharing.
Traditionally, healthcare systems function as one-to-many networks, where a single provider or organization delivers care or resources to a wide population. For instance, a hospital might distribute resources to numerous patients, but those patients are rarely directly connected to one another. The Small World Theory, however, fosters a many-to-many network where connections flow dynamically between all participants—providers, patients, and supporting entities.
This is an important innovation. In a many-to-many model, every participant becomes both a recipient and a contributor to the network.
For example, a rural patient using a telehealth platform might receive specialized care from a distant provider. At the same time, their data could inform research that benefits another patient in a different region. Similarly, a primary care doctor could collaborate with multiple specialists across the country, sharing insights that enhance care for all their patients as an integrated care team.
This many-to-many framework is transformative for healthcare accessibility. It ensures that knowledge, expertise, and resources don’t flow in one direction but are continuously shared and optimized throughout the network.
A single patient might consult a specialist in one state, connect with a pharmacist for medication in another, and join a support group for chronic disease management online—all through the same network and each provider can directly manage the outcome of a shared patient. Meanwhile, each of these connections strengthens the overall web, creating new opportunities for collaboration and innovation.
Small World Theory platforming is the how LinkedIn, Amazon, Airbnb, Experian and countless other platform networks change the behavior of their populations. Healthcare is next.
The many-to-many approach, grounded in the Small World Theory, ensures that healthcare systems become more equitable, scalable, and resilient. By leveraging the power of interconnectedness, this model dismantles barriers to access, fosters collaboration, and drives value-based care that serves both individuals and communities.
Will the healthcare system toss their outdated EMRs, their cumbersome HL7s and in-network silos for a small world model that will serve healthcare?
We’ll be watching.
Let's Talk. Jump on my calendar to discuss your case for Small World Theory.
Subscribe to edTalk for more population health perspectives.
Other Blogs
The Plan No One Sees Coming—But Soon Will
Exclusive
Mental Health
Addiction
Drugs

Ant Pheromone Study May Improve Mental Health Outcomes
Exclusive
Mental Health
Addiction
Drugs
Interrupting Violence Should Be Irresistibly Investable
Exclusive
Mental Health
Addiction
Drugs
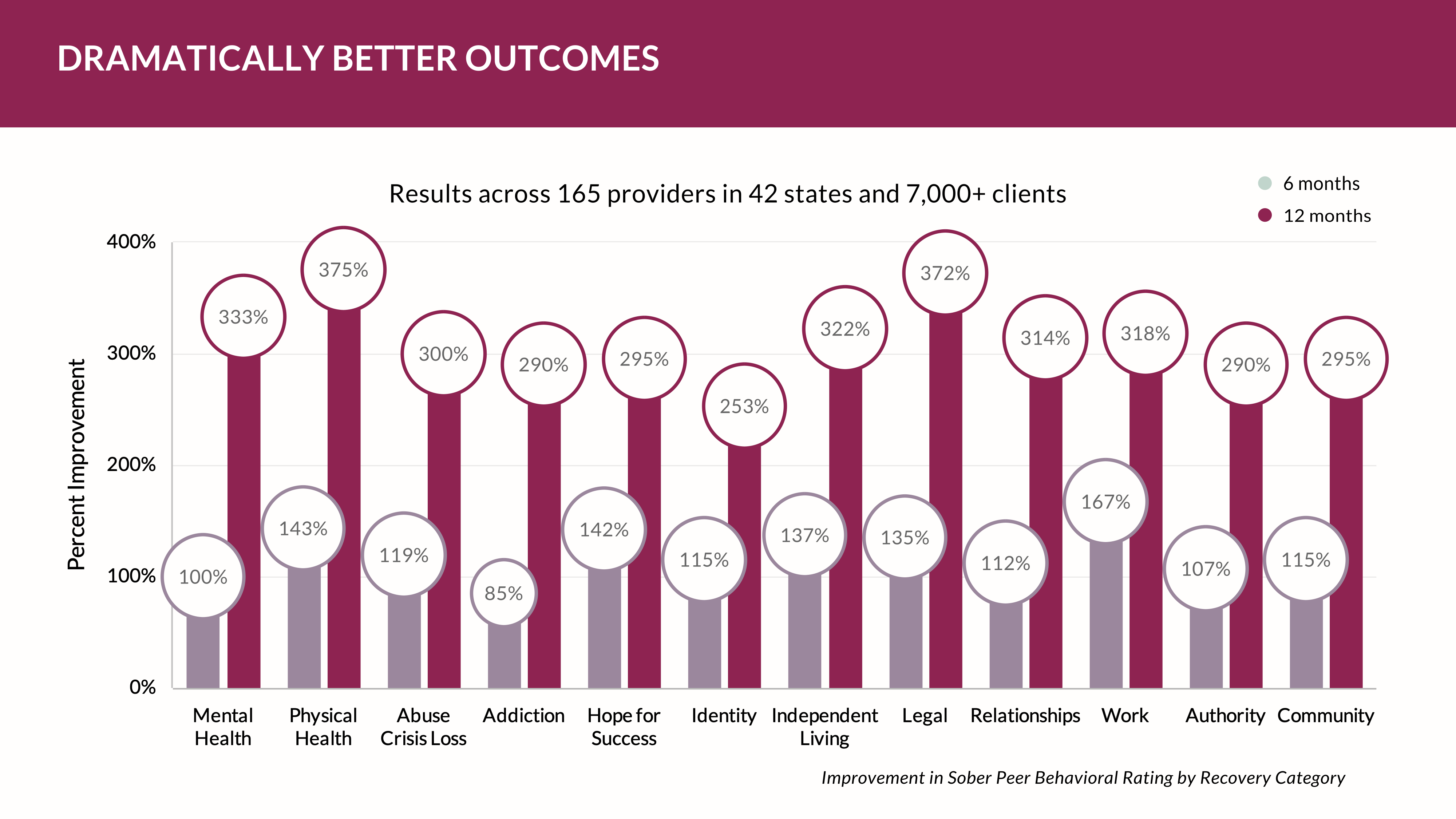
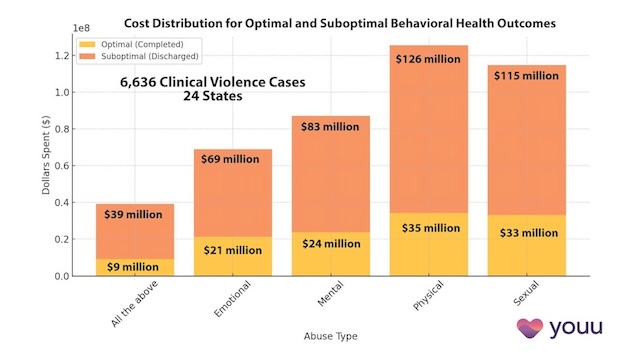
69% of Behavioral Health Patients Receive Sub-Optimal Care According to a New Analysis
Exclusive
Mental Health
Addiction
Drugs
Other Blogs
Have Questions? Lets Meet
Select a time you like to meet with us