Published Date:
Sep 28, 2023
Fee-for-service
Patients
Payer
Provider
Is Fee-for-Service driving low pay for behavioral health workers?
Selling value vs. time makes healthcare work.
Here’s what we’re watching this week on edTalk.
There’s been no shortage of ink spilled lamenting the underpaid and overworked healthcare worker. But none has garnered more attention recently than those serving the behavioral health community. Recent market intervention by government to protect mental health parity is a temporary reprieve aimed at “fairness” but its inevitable outcome could lead to a far more complicated mental health market to come.
The concept of fairness may not be that fair
The market economics of the healthcare industry is controlled by fee-for-service pricing. That’s determined by the risk-taker through “reimbursement” which, in this case, is the payer (private or public) who’s playing the value pricing game alone. The payer gets paid (from member premiums) for the value of its risk – plus its cost (the part you get as a reimbursement plus a few bucks). In the future the smartest providers will learn to play the value game themselves and take full advantage of an additional margin in exchange. Be sure to re-read that last sentence again.
Why every provider should be rushing to value pricing
Fee-for-service is currently used as a highly-controlled process to influence the market’s access — until one day soon it may not be needed. To get there, an infrastructure is needed that understands how to measure and account for value processes. More on how we do that later.
How does this marketplace affect worker pay and where are we going
According to the U.S. Bureaus of Labor & Statistics, median pay for a behavioral health worker is $48,520, requires a bachelor degree, no work experience in a related occupation or on-the-job training.
Now, here’s a comparison of other professionals – not expressed in any comparative way except median annual pay – that are customarily associated an exchange of work of 2,080 hours, annually:
$81.040. A psychologist.
$77,600. A registered nurse.
$63,000. A public defense lawyer.
$60,250. A probation officer and correctional treatment specialist.
$50,390. A social worker.
$48,520. A behavioral health worker.
$38,560. Rehab counselor.
Today providers sell their time by requesting reimbursement for it. Unfortunately, the payer figures that out for them. Remember the payer is playing the value-game alone. It alone decides who and what is paid because it’s enjoying that special multiplier called “risk”.
Don’t sell your time. Instead sell your value.
Fee for service infrastructure is essentially a price list that regulates the maximum pay for a unit of time. Selling time isn’t the most productive use of it, especially when someone else established that value for you. Ask any entrepreneur about this simple concept and they’ll tell you they don’t sell time, they sell value.
Take, for instance, the example of the public defender in the pay scale above. A private lawyer, who focuses on the value of the case makes, on average 2.5x a public defender ($168,000 vs $63,000). The public defender, of course, works on a fee-for-service arrangement per case. Obviously not wanting to lose a case, the defender isn’t assuming the reputational risk of a private lawyer. That risk is priced into the private lawyers much higher rate of pay. The same concept goes for most any profession operating on a fee-for-service basis.
How do we finally get to higher wages, better value and care?
Improving our healthcare system to deliver better quality care at lower cost is critically important to our nation’s long-term economic and fiscal wellbeing. In 2021, the U.S. devoted 18 percent of its economy to healthcare. Such a large proportion of resources devoted to healthcare makes it increasingly difficult to invest in other sectors of our economy.
It’s going to take a new kind of infrastructure for transformation. The consulting firm McKinsey & Company agrees. New, value based platforms designed for the job are going to be the big players to pull it all together in healthcare’s future.
In their book “Business of Platforms” authors Michael Cusumano, Annabelle Gawer and David Yoffle break the new infrastructure down this way;
“Platforms are unique businesses driven by network effects and multisided market dynamics.”
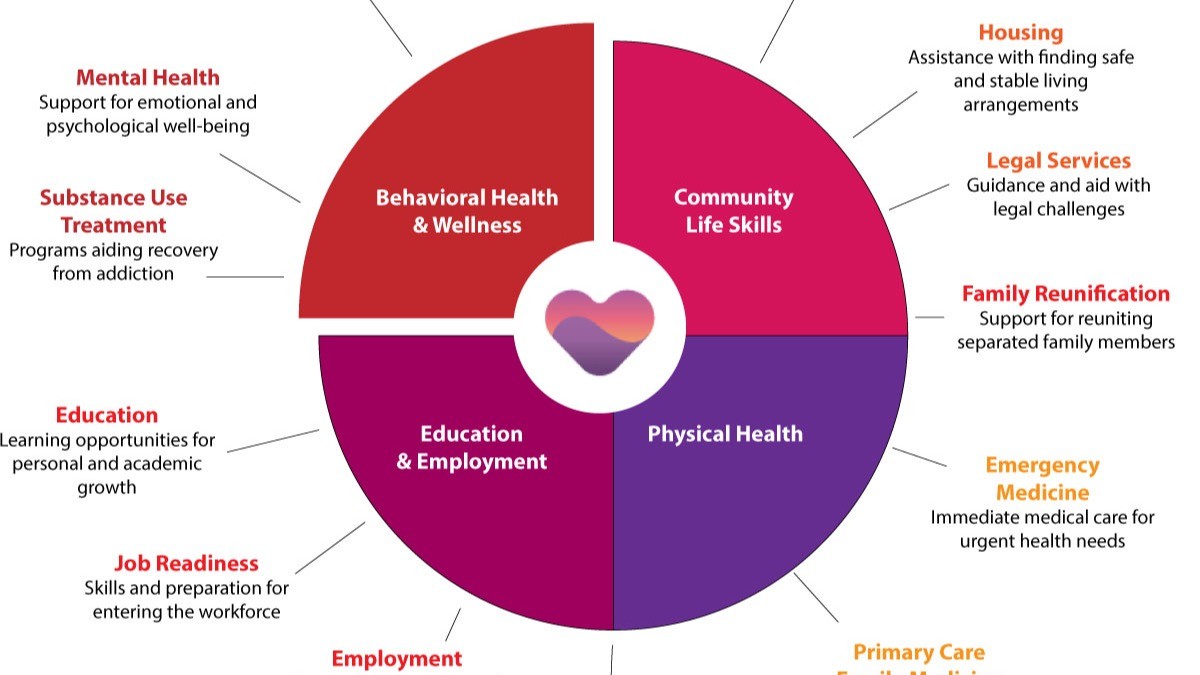
Much like Amazon which controls both buyers and sellers in a hybrid central platform, for instance, their platform acts as a centralized hybrid repository. Think of Amazon as a super-switch that controls both the price and profit potential based on the availability of products and services. In healthcare, new super-switched platforms are emerging like YOUU Health where services and providers connect to maximize value (full disclosure, our office developed and owns this hybrid platform).
On one side sits providers who deliver services (called transactors). On the other are all the tools used by them (like EHR’s, AI, digital health, etc. called innovations) freely connecting to the tools needed for day-to-day provider-delivered care. Cross connectivity of care team to other providers and their inter-connected patient data are shared anywhere.
We’ve discussed the regulatory forecast setting up this future vision in another edTalk here.
Of course, there is no guarantee that our industry will be treated equally or fairly by breaking away from fee-for-service, as the market normally allows for competition to drive prices and wages. It is going to be interesting to see our behavioral health actors learn how to participate in the new value-based market, improve their profits and give our worker’s a well-deserved, and “fair” pay rate.
We’ll be watching.
_____________________________________________________
And, in the meantime we’ll be listening and talking edTalk. See you next time.
Don’t forget to subscribe.
Other Blogs
The Plan No One Sees Coming—But Soon Will
Exclusive
Mental Health
Addiction
Drugs

Ant Pheromone Study May Improve Mental Health Outcomes
Exclusive
Mental Health
Addiction
Drugs
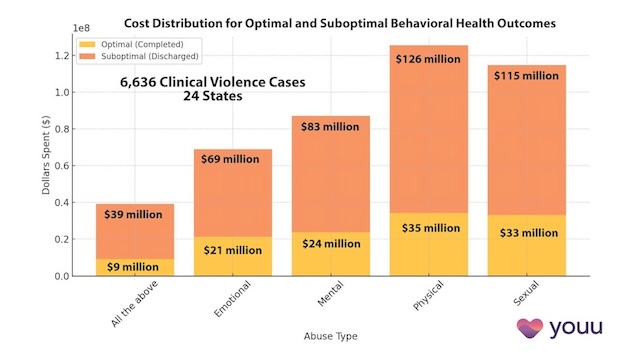
Interrupting Violence Should Be Irresistibly Investable
Exclusive
Mental Health
Addiction
Drugs
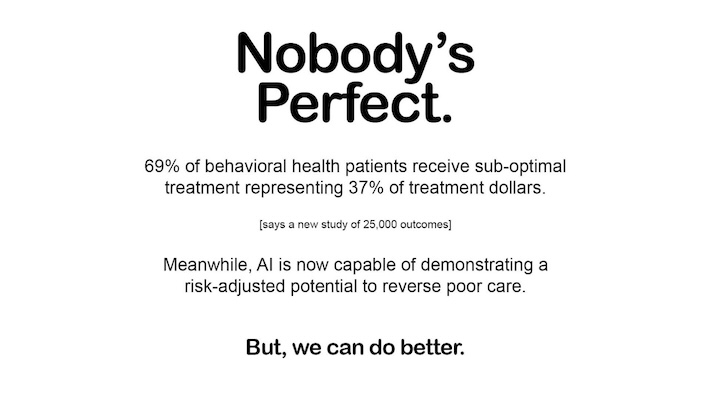
69% of Behavioral Health Patients Receive Sub-Optimal Care According to a New Analysis
Exclusive
Mental Health
Addiction
Drugs
Other Blogs
Have Questions? Lets Meet
Select a time you like to meet with us