Published Date:
Oct 2, 2024
Exclusive
Mental Health
Addiction
Drugs
How Payers Are Using AI to Outpace Manual Claims
How Payers Are Using AI to Outpace Manual Claims
A new and critical challenge is emerging in the world of revenue cycle management (RCM): insurance companies, or payers, are leveraging AI and automated systems to process and deny claims at unprecedented levels.
This development is placing enormous pressure on healthcare providers, particularly those relying on providers using third-party billing firms that still process claims manually. The rise of AI-driven payers has made it clear that the days of slow, manual claims management are numbered. Providers must adapt by dramatically improving the quality and integration of their
electronic health record (EHR) systems to the billing process to the revenue cycle workflows.
Health is largely a billing process burdened by inefficiencies. Manual claims are sent in by third-party billing firms, often riddled with small errors or lacking key details. In many cases, these errors would result in claim denials or significant delays in payment. However, as AI technology has evolved, payers have become more sophisticated in catching these errors. AI bots can now scan claims for issues much faster than any human workforce, leading to more frequent and rapid denials. This is creating a significant burden for providers, as their cash flow becomes disrupted and claims are left unpaid or delayed.
The rise of payer AI has made one thing clear: hospitals and healthcare organizations can no longer rely on outdated billing systems or manual processes. To keep pace with AI-driven payers, healthcare providers need to produce cleaner, higher-quality claims that can survive the scrutiny of automated systems. This means a much tighter integration between electronic health records (EHRs) and the billing process, ensuring that claims are automatically generated with accurate and comprehensive data.
In many organizations, the EHR has historically been seen as a clinical tool —designed to store patient records, track treatments, and monitor outcomes. But in today’s healthcare environment, it needs to serve as much more than that. The EHR must become the backbone of the revenue cycle, producing claims that are not only detailed but also fully integrated with the provider's financial and billing systems. The key is to automate as much of the claims process as possible, using advanced algorithms to ensure that all necessary data is included and properly formatted before the claim is ever sent.
The push for automation is especially urgent for third-party billing firms, which are often more reliant on manual processes. Many of these firms lack the sophisticated EHR integration needed to compete with the AI bots being deployed by insurance companies. As a result, they are seeing more frequent denials and falling behind in collecting payments. To remain viable,
providers must embrace automation so that their systems are capable of producing the high-quality claims that payers now demand.
In addition to improved claim quality, automation can help address another key issue: compliance with constantly changing healthcare regulations. The healthcare landscape is always shifting, with new policies and requirements emerging at both the federal and state levels. AI-driven payers are quick to adapt to these changes, often denying claims based on the latest regulations. To avoid revenue losses, healthcare providers must be just as agile, using their integrated EHR systems to ensure that claims meet all regulatory requirements before submission.
The path forward is clear. As payers continue to deploy AI to process and deny claims, healthcare providers must adapt by improving their technology. The future of healthcare finance depends on tighter EHR integration, automation, and a commitment to producing higher-quality claims. Those that succeed in this transition will not only stay competitive but will also ensure the financial stability needed to continue providing excellent patient care.
The time for innovation is now—before the AI bots deployed by payers make manual claims management a thing of the past.
Other Blogs
The Plan No One Sees Coming—But Soon Will
Exclusive
Mental Health
Addiction
Drugs

Ant Pheromone Study May Improve Mental Health Outcomes
Exclusive
Mental Health
Addiction
Drugs
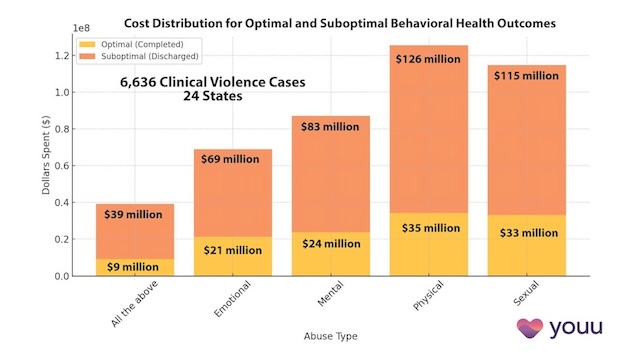
Interrupting Violence Should Be Irresistibly Investable
Exclusive
Mental Health
Addiction
Drugs
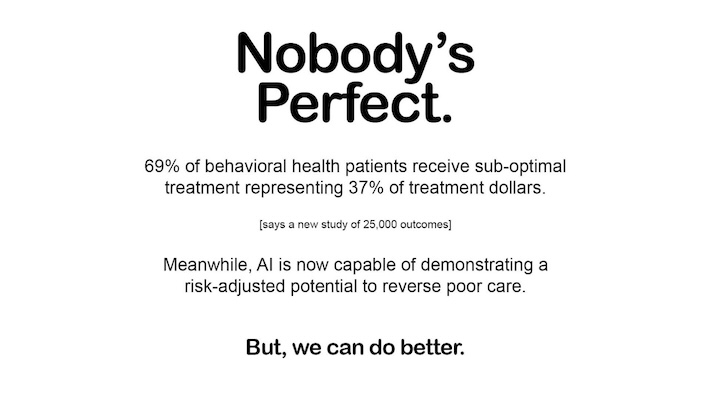
69% of Behavioral Health Patients Receive Sub-Optimal Care According to a New Analysis
Exclusive
Mental Health
Addiction
Drugs
Other Blogs
Have Questions? Lets Meet
Select a time you like to meet with us