Published Date:
Dec 10, 2024
Exclusive
Mental Health
Addiction
Drugs
Healthcare Payment Reform is Around the Corner
Will adopting a hybrid payment model and addressing the imbalances in the current valuation process, and the Pay PCPs Act offer a promising path forward?
If current legislation is successful, the behavioral health industry could benefit from payment reform which is likely to be birthed in the primary care sector – and spread to promise a more integrated solution for patients affected by mental health or substance use disorders. Here’s an overview of the payment reform landscape every provider should be watching.
The healthcare landscape is at a pivotal moment. The introduction of the Pay PCPs Act signals a bipartisan commitment to addressing long-standing issues within payment structures.
The Flaws of the Fee-for-Service Model
The FFS model inherently incentivizes quantity over quality. Physicians are motivated to see more patients and provide more services, sometimes at the expense of personalized, patient-centered care. This system lacks the flexibility for physicians to spend the necessary time with each patient, coordinate care effectively, or focus on preventive measures that keep patients healthy in the long term. Over time, this has led to an overemphasis on specialty care, which is often more expensive, while primary care—the backbone of a robust healthcare system—remains underfunded and undervalued.
A Promising Alternative: The Pay PCPs Act
Recognizing these challenges, Senators Sheldon Whitehouse (D-RI) and Bill Cassidy (R-LA) have introduced the Pay Primary Care Physicians (Pay PCPs) Act. This bipartisan legislation aims to reform how primary care physicians are compensated, introducing a "hybrid" payment model that blends traditional FFS payments with population-based payments.
Here's How a Hybrid Payment Model Will Work
Under the proposed hybrid model, primary care physicians would receive two types of payments:
1. Population-Based Payments: A per-patient, per-month payment that covers a core set of services, including care management, coordination, telehealth, and other high-volume, low-cost services. This approach provides a steady revenue stream and the flexibility to focus on comprehensive care without the pressure to increase service volume unnecessarily.
2. Fee-for-Service Payments: Traditional payments for services not covered under the population-based payment, ensuring that physicians are still compensated for additional necessary procedures and treatments.
Research suggests that 60% to 70% of payments for most primary care clinicians could be covered by the new population-based payment. By providing a significant portion of income through this model, physicians can invest more time and resources into personalized care, preventive measures, and care coordination.
Addressing Payment Imbalances
Another critical component of the Pay PCPs Act is the establishment of a Technical Advisory Committee (TAC). This committee would advise the Centers for Medicare & Medicaid Services (CMS) on the valuation of services in the Medicare physician fee schedule. Currently, the process for determining these valuations heavily relies on recommendations from the American Medical Association (AMA)/Specialty Society Relative Value Scale Update Committee (RUC).
While the RUC plays a significant role, there's a growing concern that its recommendations contribute to the overvaluation of specialty services and the undervaluation of primary care and other core care services.
By creating the TAC, the legislation seeks to bring more transparency, independence, and balance to the valuation process. This could lead to more equitable compensation for primary care services and encourage more physicians to enter and remain in primary care fields.
Support and Recommendations
Make Hybrid Payments the Default: Advocate for the hybrid capitated payment model to become the default for primary care, pushing the healthcare system further away from the limitations of FFS.
Set Payment Proportions with Flexibility: Encourage Congress to stipulate a range for the population-based payment proportion, ensuring a sufficient floor so CMS can fine-tune the payment structure effectively.
Improve Data Collection and Transparency: Urge CMS to implement accurate and ongoing data collection to independently validate recommendations from the RUC and improve transparency in how valuations are determined.
Ensure medical records systems are adaptable: to these new payment models and the technology needed to manage patient navigation and accounting.
Where do we go from here
Reforming how primary care physicians are compensated is an important step toward a more efficient and patient-centered healthcare system.
Will adopting a hybrid payment model and addressing the imbalances in the current valuation process, and the Pay PCPs Act offer a promising path forward?
We'll be watching.
About the Author: Ed DeShields
Ed DeShields is Chairman of Community Assurance and Chairman of YOUU Health, a powerfully interconnected healthcare navigation platform.
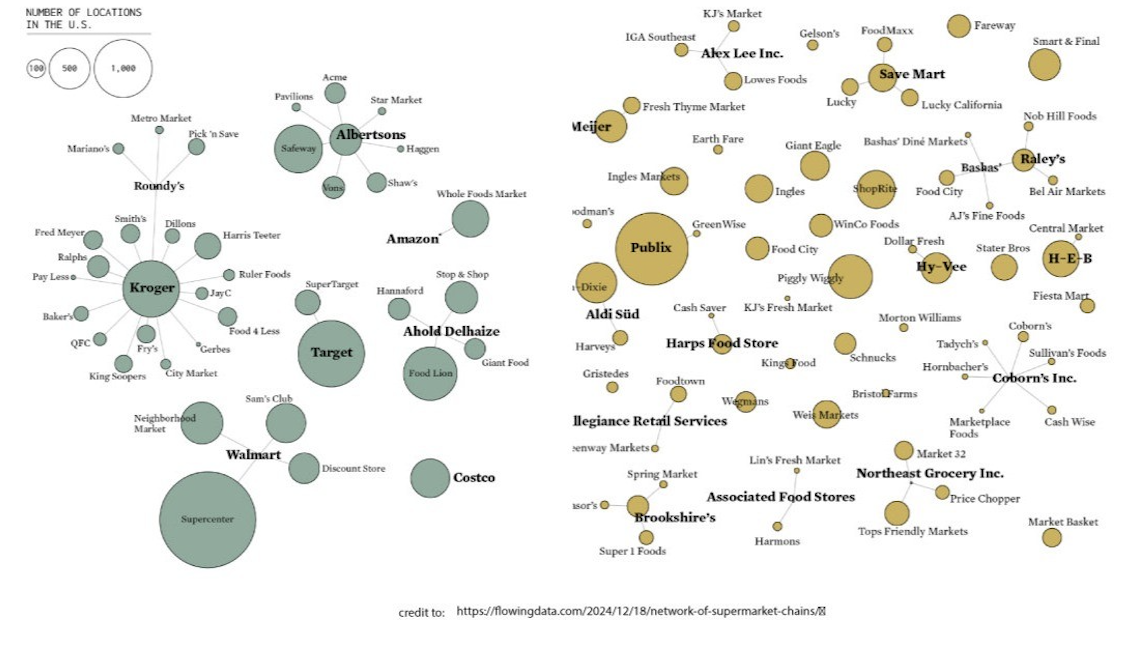
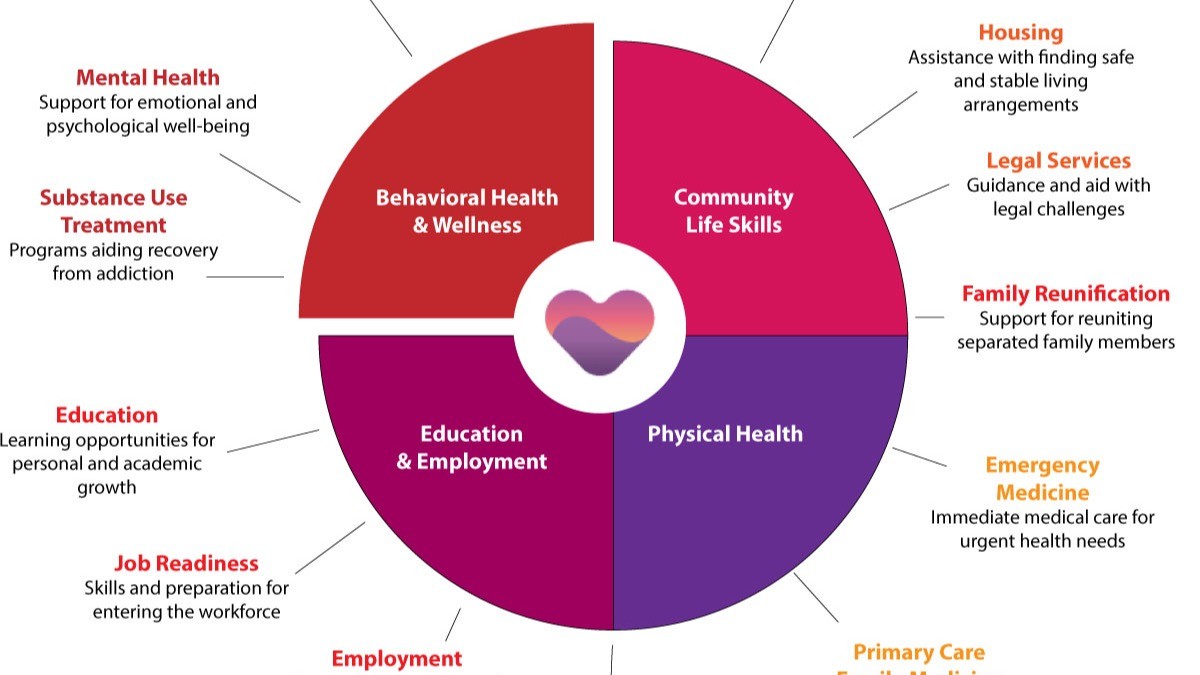
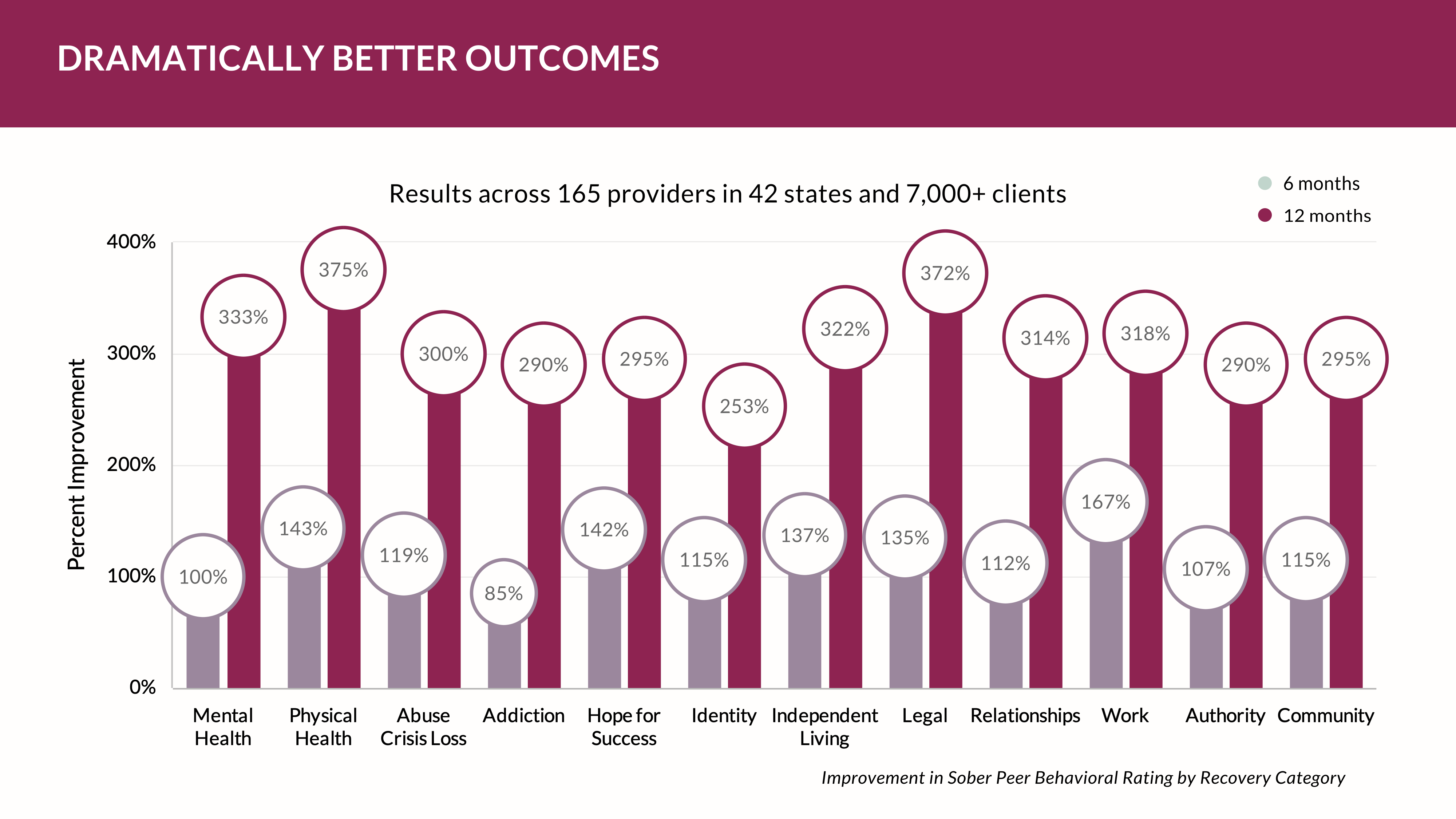
The YOUUniverse, is our hyper-connected network health cloud allows you to quickly build your healthcare community across any care continuum for the life of the patient. Connect to any provider or care team anywhere - in one platform - to navigate or coordinate care for your patient with ease; then, wrap it with the important revenue driving and clinical outcome producing workflows.
For more information on the YOUUniverse for your practice visit YOUU.com or for a demonstration or discussion please visit our calendar HERE.
Other Blogs
The Plan No One Sees Coming—But Soon Will
Exclusive
Mental Health
Addiction
Drugs

Ant Pheromone Study May Improve Mental Health Outcomes
Exclusive
Mental Health
Addiction
Drugs
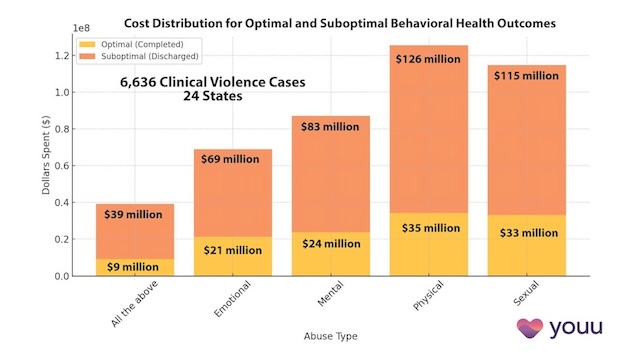
Interrupting Violence Should Be Irresistibly Investable
Exclusive
Mental Health
Addiction
Drugs
69% of Behavioral Health Patients Receive Sub-Optimal Care According to a New Analysis
Exclusive
Mental Health
Addiction
Drugs
Other Blogs
Have Questions? Lets Meet
Select a time you like to meet with us