Published Date:
Apr 30, 2024
Exclusive
Mental Health
Addiction
Drugs
Healthcare Needs a Social Capital Model
The network effect of hyper-localized healthcare will save your practice and drive better results.

Healthcare Needs a Social Capital Model
The network effect of hyper-localized healthcare will save your practice and drive better results
More than three-quarters of the healthcare workforce in “traditional” roles —especially frontline care workers and clinicians— report they are connecting with others less frequently. According to recent survey data, healthcare workers have disproportionally smaller networks and spend less time and effort on relationship building across referral or care networks. This decline is concerning. As their world shrinks myopically into a volume-driven fee-for-service model, it’s almost universally agreed that it’s harder to keep healthcare sustainable.
Simultaneously, the attrition of healthcare workers and hiring challenges are predictable. Patient’s lack of access to behavioral health and haphazard chronic care navigation are its unintended casualty. But there is a solution, so says the consulting giant McKinsey & Company.
Social Capital Model: Improving practice and patient performance
The solution may lie with a renewed sense of social capital and a well-known community model called the Network Effect—or the intentional development of expanded formal networks, relationships, shared norms, and trust among individuals, teams, and patients outside the small world of today’s siloed service offerings. Simply put, we need more social connectivity with our colleagues for team care; in the community where the patients have convenient access to it.
At its core, the theory behind Network Effects suggests that platforms and services using network effects get better as they get bigger — not just in value to users, but also in accruing more resources to improve their potential outcome, thus strengthening the “flywheel” of improvement.
But, as is commonly the case, the lack of capital to build social connectivity is uneven across industries. For example, about 30 percent of employees in the banking and technology sectors report having more contact with their networks in the last two years. By contrast, fewer than 10 percent of employees in healthcare report the same.
Moreover, only 9 percent of frontline workers report feeling more connected with their networks over the past few years, compared with 22 percent of middle managers and 45 percent of senior leaders.
In the current healthcare environment, referrals, personal connections, and perceptions of how inclusive and communal a practice looms ever larger with a patient’s decision about where to look for care. A common refrain for most behavioral health practices is social media SEO advertising instead. SEO is expensive and adds a layer of cost to an already cost-burdened practice.
Social capitalization is quite different. It implies that practice leaders better manage social capitalization in the same way they manage financial, human, and other forms of corporate capital: to build interconnected care teams systematically and intentionally in and out of their existing network.
The Social Capital Model Visualized
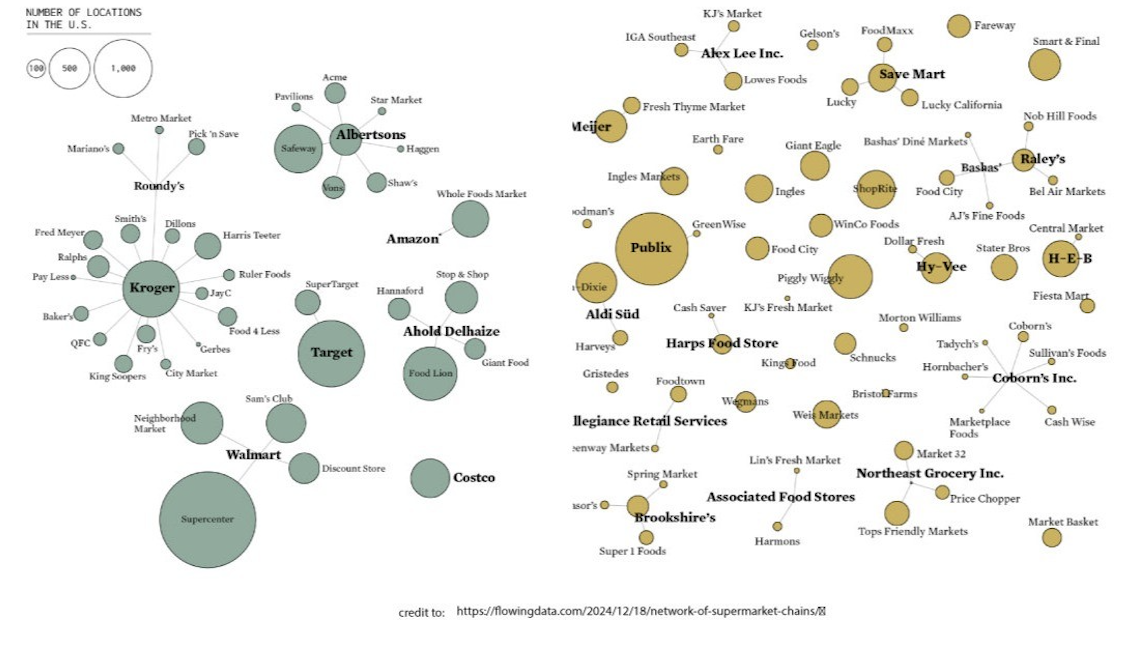
Consider the following geographical community map in Figure 1.
Let’s look at the numbers. The map here shows a representative example of Orange County, California. It perfectly illustrates the behavioral health Network Effect. Each dot represents a community of clinical or non-clinical referral sources (i.e. providers) serving this hyper-local market.
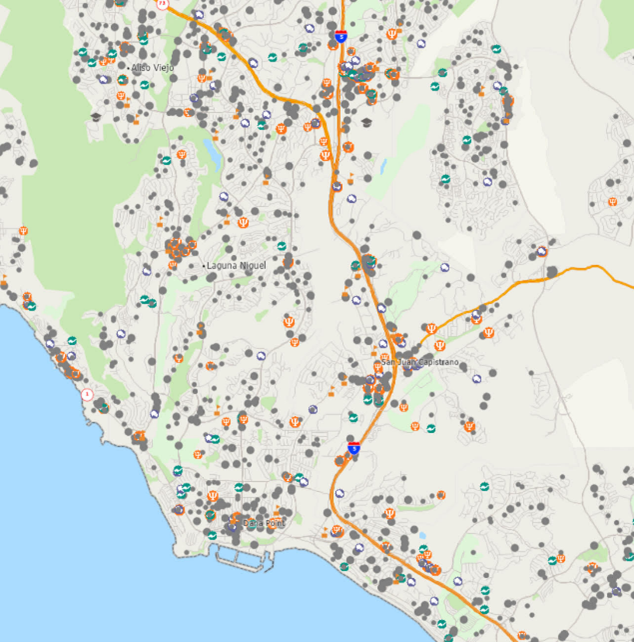
This map includes:
Primary Care
Psychologists
Clinical Behavioral Health Facilities
County Health Departments
Court and Correctional Institutions
Homeless Shelters
Charitable Assistance Organizations
K1-16 Education, Colleges & Universities
Hospitals and Clinics
Churches and Places of Worship programs
In other words, they are the front-door of care. The more dots connected to your social capital map the greater the exponential possibilities for practice growth.
Here’s an example. PCP ambulatory care visits with a behavioral health diagnosis have a very high probability of referral to higher value specialized care. In fact, one in twenty-nine (1:29) PCP visits culminate with behavioral health as the primary diagnosis. Understanding PCP referral patterns for patients with behavioral health conditions is essential to access and care navigation/coordination. Thus, there’s ample opportunity to deliver a high-value interconnected specialty service, that is, if you’ve built an interconnected social network to this PCP.
Let’s quantify what I’m talking about; there are one-half a billion patient visits to a PCP each year and 3.4% of them are going to get referred to a behavioral health provider. That’s 17,000,000 patients going somewhere for help – or not. I’ll note that these aren’t leads from an internet CRM/SEO internet advertising campaign. They’re professional referrals within a direct accountable care relationship that are the beginning of a high-value care team relationship.
When behavioral health providers operate in an interdisciplinary care team relationship they will someday propel behavioral health into a new starring role as a high-value specialty. They’ll lock the patient into a disciplined life-cycle journey of recovery to measure it and predict future patient risk where a high-value offering will be born.
So where do we go from here?
You can start by assessing your own social capital along three dimensions:
Motivation. Is your practice motivated to build and maintain relationships, and are you in an environment that encourages such relationship building?
Access. Does your practice have access to the outside networks and relationships you are looking to build?
Ability. Have you invested in a network effect platform and do your employees have what they need (such as time, resources, and skills) to build and maintain those networks and relationships?
As mentioned above, the power of Network Effect suggests that platforms and services using network effects get better as they get bigger. That’s connecting the dots to develop an intentional social capital model for your practice.
But will behavioral health emerge from its malaise to build its social capital and lead with a network effect community?
____________
We’ll be watching.
And, in the meantime we'll be listening and talking edTalk. See you next time.
About YOUU Health
YOUU Health is the most powerfully interconnected healthcare navigation platform ever.
Our hyper-connected network effect health cloud allows you to quickly build your healthcare community across any care continuum for the life of the patient. Connect to any provider or care team anywhere - in one platform - to navigate or coordinate care for your patient with ease. Then, wrap it with the important revenue driving and clinical outcome producing workflows. You'll be amazed how easy it is to build a thriving practice. For more information on the YOUUniverse for your practice visit YOUU.com or for a demonstration or discussion please visit our calendar HERE.
Other Blogs
The Plan No One Sees Coming—But Soon Will
Exclusive
Mental Health
Addiction
Drugs

Ant Pheromone Study May Improve Mental Health Outcomes
Exclusive
Mental Health
Addiction
Drugs
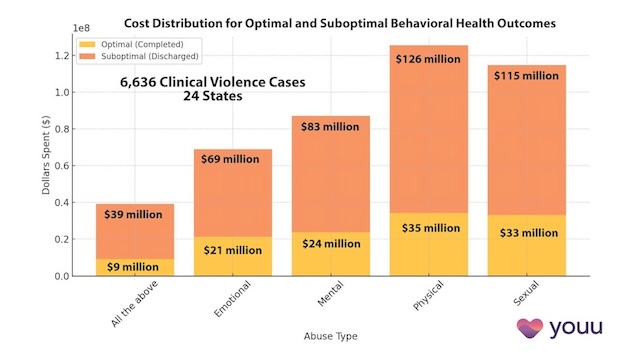
Interrupting Violence Should Be Irresistibly Investable
Exclusive
Mental Health
Addiction
Drugs
69% of Behavioral Health Patients Receive Sub-Optimal Care According to a New Analysis
Exclusive
Mental Health
Addiction
Drugs
Other Blogs
Have Questions? Lets Meet
Select a time you like to meet with us