Published Date:
Sep 28, 2023
Behavioral health
healthcare
Value-Based Care
PCP
Can Behavioral Health Emerge As Healthcare’s Most Valuable Care Specialty?
There’s a lot of evidence out there to support the thesis that behavioral health could emerge as a high-value care specialty.
Here's what we're watching this week at edTalk.
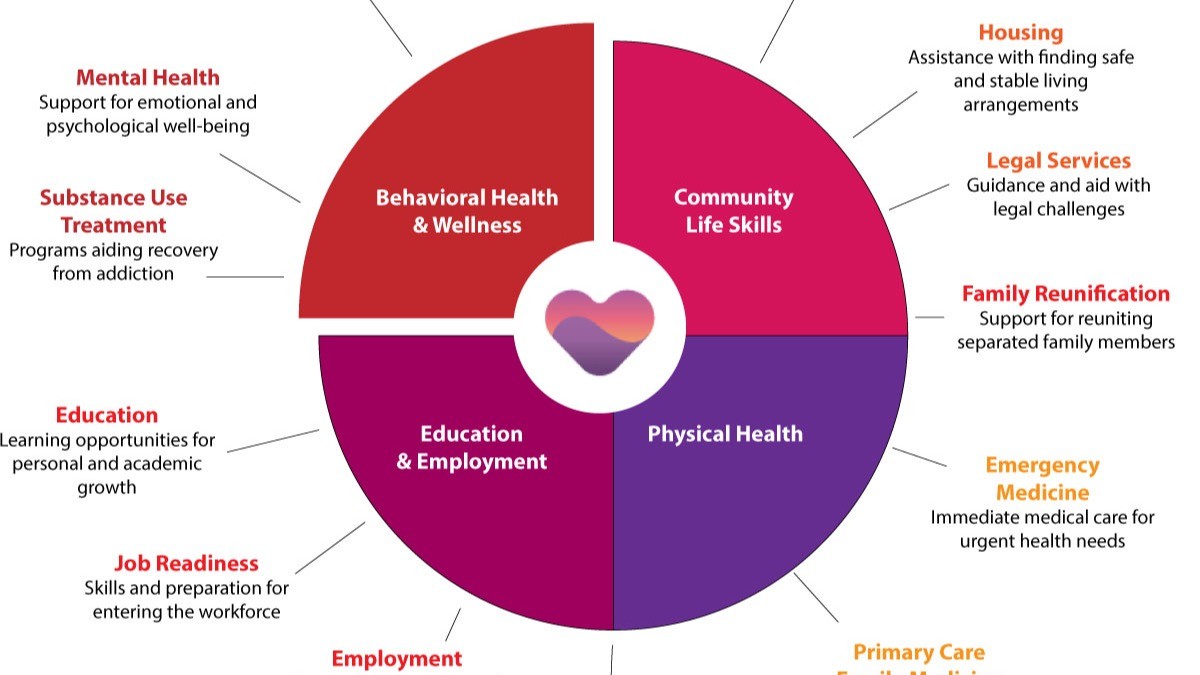
Behavioral health is a lot of things, but at the top of this list is the fact that people can reduce their risk of developing major medical problems, receive more effective treatment, and reduce their health care cost when they seek treatment from a team featuring behavioral health.
There’s a lot of evidence out there to support the thesis that behavioral health could emerge as a high-value care specialty.
The promise of integrating cross-discipline care teams raises the value proposition for health plans as we move to a value-based economic model. Most importantly, bolstering integration into the mainstream healthcare market raises its total addressable market to sixty percent (60%) of total healthcare spend of the insured member market in the U.S.
Read the tea leaves. The market for integrated approaches is fluid and robust. For example, the expansion of behavioral health service delivery by home care companies is making big advances as Amerdidys, Elara Caring and Bayada Home Health are predicting 7%-25% of their revenue mix to include behavioral health.
But, far and away the most important pathway to behavioral health is the referral from the primary care physician (PCP).
Let’s look at the numbers.
PCP ambulatory care visits with a behavioral health diagnosis have a very high probability of referral to higher value specialized care. In fact, one in twenty-nine (1:29) visits to a PCP concludes with behavioral health as the primary diagnosis. Understanding PCP referral patterns for patients with behavioral health conditions is essential to access and care coordination. If PCPs are unable to adequately manage the patient’s clinical needs, then referrals become a necessary part of providing high-quality care. Thus, there’s ample opportunity to deliver a high-value interconnected specialty service.
Let’s quantify what I’m talking about; there are one-half a billion patient visits to a PCP each year and 3.4% of them are going to get referred to a behavioral health provider. That’s 17,000,000 folks going somewhere for help – or not. I’ll note that these aren’t leads scrapped from the internet. They’re professional referrals within a direct accountable care relationship that are the beginning of a high-value care team relationship.
If you consider only the insured population, it’s even more impactful. Twenty-three percent (23%) of all insured members have been diagnosed with a BH diagnosis at one time or another. That translates to a seven percent (7%) spend on members being treated for it and a whopping fifty-three percent (53%) spend on a co-occurring health issue for other medical services.
As the math clearly points out, sixty percent (60%) of health expenditures are spent for members with an associated behavioral health problem.
That’s a naturally correlated integration isn’t it! Thus, we have a disproportional driver of healthcare’s catastrophically rising costs and a major contributor for why healthcare is unaffordable. This inefficiency is picking the pocket of the provider and the payer.
Our infrastructure and will-to-change is going to create vast new value
The fact that only fifty-percent (50%) of our behavioral health providers have considered investing in an electronic healthcare record system can only be described as a Jed Clampett moment; “that’s pit-i-ful”. But to their credit, today’s EHR hasn’t exactly evolved into a infrastructure that promotes high-value. Here’s some facts.
According to a Stanford Medical School study:
· 40% of providers say the EHR presents more challenges than benefits.
· 49% think they distract from clinical effectiveness.
· 50% think they should be completely overhauled.
· 62% of time is spent in the EHR and not with the patient.
· 67% believe inter-operability between providers should be a top priority.
· 71% think their EHR is leading to workplace burn-out.
· 92% know that their EHR is not a clinical tool.
So healthcare is in the early stages of an extraordinary change preparing for a wholesale change to its tech infrastructure where the old EHR will be largely left behind.
Tomorrow’s emerging Gen3 value-based tech-infrastructure is going to pull this together – at less cost and complexity.
So what’s next?
It’s going to put the focus back on super-star value and premium specialty services for behavioral health providers.
When behavioral health providers operate in an interdisciplinary care team relationship – like an accountable care organization – they will someday propel behavioral health into a new starring role as a high-value specialty. They’ll lock the patient into a disciplined life-cycle journey of recovery to measure it and predict future patient risk where a high-value offering will be born.
So, for you superstars of innovation, you imaginative creators of value, press on. The facts make it clear, behavioral health has it all. It has scale, access, and value. But will behavioral health emerge from its malaise to become healthcare’s most valuable care specialty?
We’ll be watching.
And, in the meantime we'll be listening and talking edTalk. See you next time.
Other Blogs
The Plan No One Sees Coming—But Soon Will
Exclusive
Mental Health
Addiction
Drugs

Ant Pheromone Study May Improve Mental Health Outcomes
Exclusive
Mental Health
Addiction
Drugs
Interrupting Violence Should Be Irresistibly Investable
Exclusive
Mental Health
Addiction
Drugs
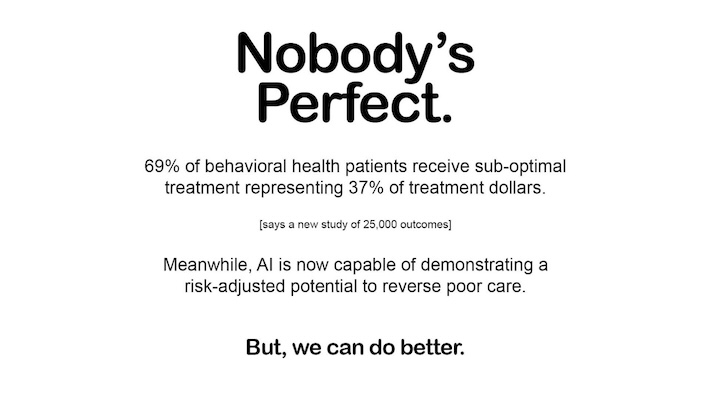
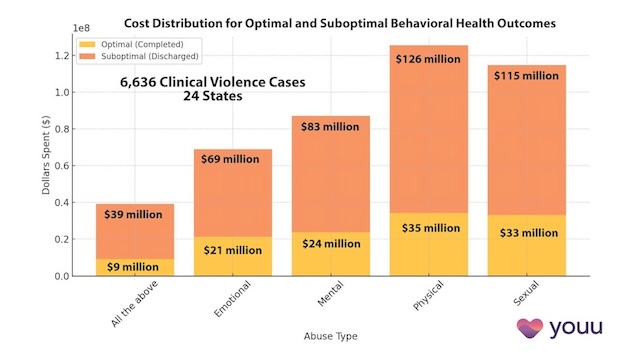
69% of Behavioral Health Patients Receive Sub-Optimal Care According to a New Analysis
Exclusive
Mental Health
Addiction
Drugs
Other Blogs
Have Questions? Lets Meet
Select a time you like to meet with us