Published Date:
Sep 28, 2023
Patient-Centered Care
Treatment
Augmentation
Behavioral Health
Are we entering an era of great clinical augmentation?
Why a clinicians' viewpoint always works better with longitudinal patient reported data
Here’s what we’re watching this week on edTalk.
Imagine living with an undetected behavioral health condition, not exactly knowing what you don't know. The negative consequence is prolonged suffering and potential complications. Conversely, the positive consequence of discovery can bring relief, treatment, and the chance for a better quality of life.
I’ve had several recent conversations, some seemingly more debate than not, about the hesitancy of behavioral health clinicians to consider the value of patient reported data. In particular, a discussion often ensues about longitudinal patient data being invalid in one way or another. But, there’s plenty of evidence to acknowledge the potential benefits this data can bring to our behavioral health workforce. So, with one eyebrow raised and an open mind, here’s my counter argument.
Patient reported data can augment a clinicians' viewpoint, and help find hidden diagnoses, providing them with a deeper understanding, particularly considering the limitations of clinicians gathering long-term longitudinal data for chronic conditions.
Let’s explore five reasons we have entered an Era of Great Clinical Augmentation.
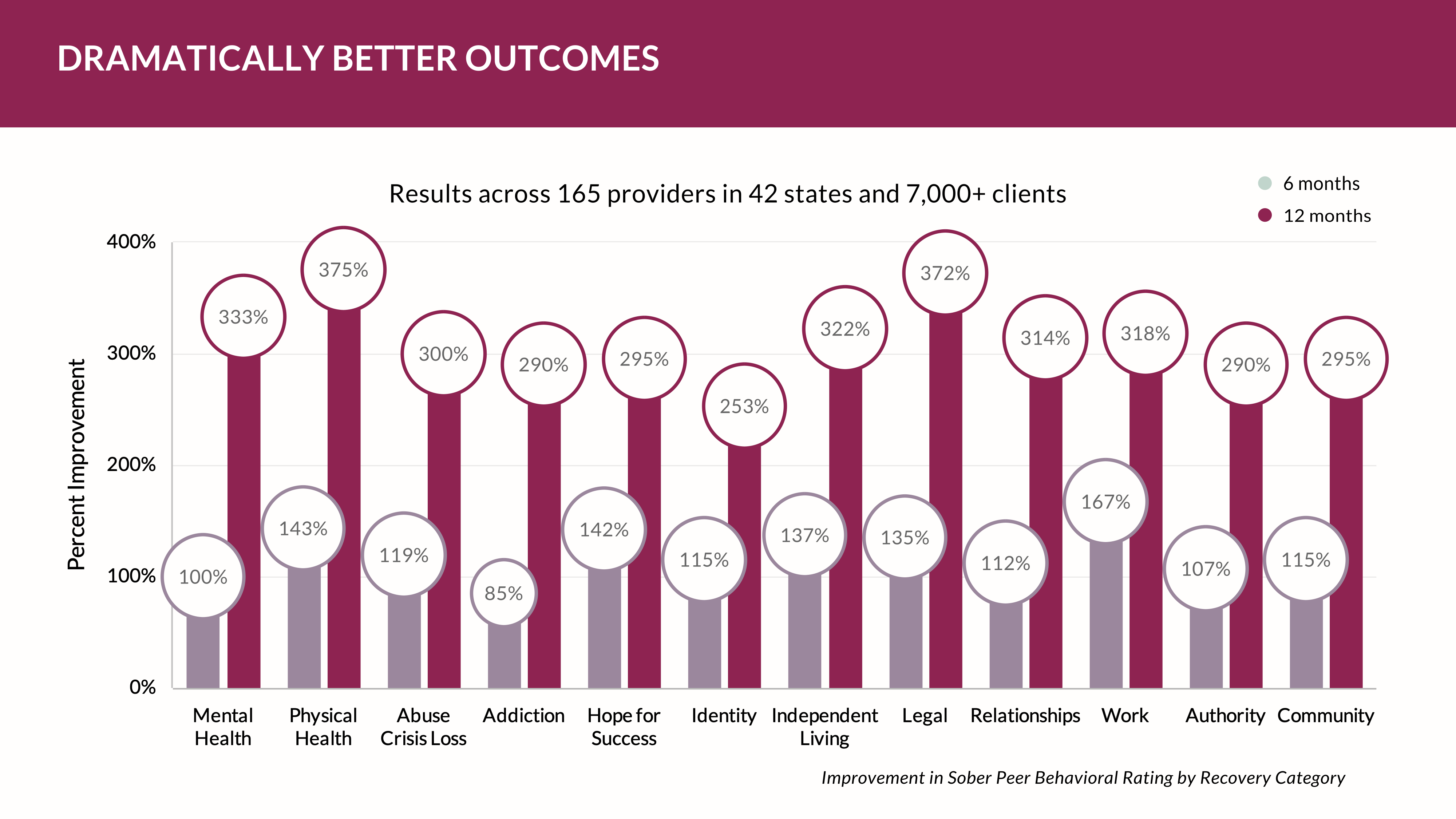
Here’s a real-life example from a YOUU Health study. From 2020-2023, YOUU Health looked at about 3.3 million longitudinal days of behavioral health clients in recovery. These data represented about 22,538 clients where we simply allowed them to independently answer 1,104,400 questions about themselves using questions often asked by clinicians without the clinician present. In addition, the patient was encouraged to journal about their feelings. Here's what we found.
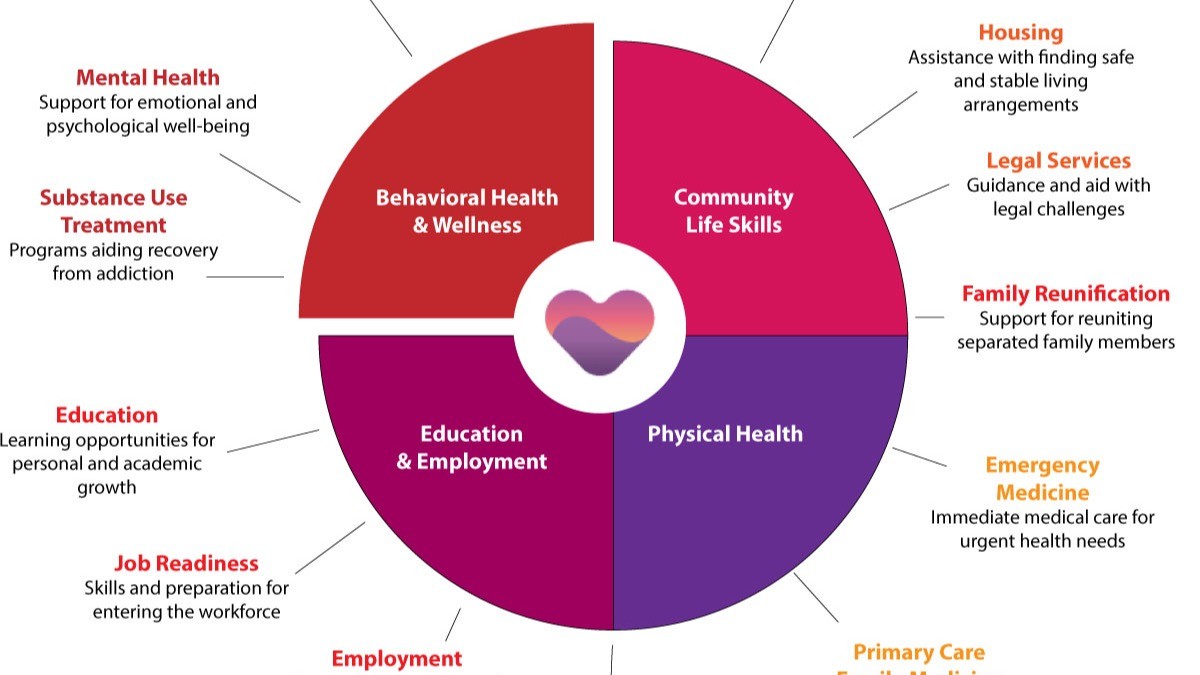
First, there’s enhanced patient-centered care.
Incorporating patient reported data allowed our YOUU Network providers to adopt a more patient-centered approach. By actively involving patients in their own care and valuing their subjective experiences, our clinician partners gained insights into the lived realities of individuals with chronic conditions. And, the patients told us they really liked the opportunity to be heard -- in their own voice.
This data provides a more comprehensive understanding of patients' symptoms, challenges, and treatment outcomes, leading to tailored and effective interventions.
Second, there’s a much richer holistic assessment of the patient’s symptoms.
Clinicians often rely on their own observations and assessments during short clinical encounters. However, these patients reported data that offered a more holistic view of symptoms, capturing variations in severity, frequency, and impact on daily functioning over time. This information helped clinicians identify patterns, triggers, and factors influencing symptom exacerbation or improvement, leading to more accurate diagnoses and targeted treatment plans.
Third, there’s greater insight for improved treatment planning.
Long-term longitudinal care for chronic conditions requires ongoing monitoring and adjustment of treatment plans. Patient reported data provided valuable information about treatment effectiveness, side effects, and adherence. Clinicians leveraged this data to make informed decisions, considering patients' perspectives and preferences, ultimately leading to more personalized and effective interventions.
Fourth, unreported concerns were spotted.
Some patients hesitate to disclose certain symptoms or concerns during face-to-face clinical encounters due to various reasons, such as embarrassment, fear of stigma, or limited time. Patient reported data platforms encourages patients to report their experiences more freely and comprehensively. This enables the clinicians workforce to uncover unreported concerns, facilitating early intervention and preventing potential complications.
Fifth, longitudinal insights and trends were established.
Clinicians who provided long-term longitudinal care faced challenges in capturing the dynamic nature of chronic conditions over time. Patient reported data, collected at regular intervals, offered valuable longitudinal insights and trend analysis. Clinicians identified fluctuations in symptoms, treatment responses, and quality of life, allowing for proactive management and adjustments in care plans.
Conclusion:
While clinicians may face limitations in providing long-term longitudinal care for chronic conditions, the integration of patient reported data significantly augmented their viewpoints and understanding. The utilization of this data enabled enhanced patient-centered care, holistic symptom assessment, improved treatment planning, identification of unreported concerns, and longitudinal insights.
So will our behavioral health workforce embrace patient reported data so clinicians can bridge the gap between episodic clinical encounters and gain a deeper understanding of patients' experiences, ultimately leading to more effective and comprehensive care?
We’ll be watching.
And, in the meantime, we’ll be listening and talking edTalk. See you next time.
Don’t forget to subscribe.
Other Blogs
The Plan No One Sees Coming—But Soon Will
Exclusive
Mental Health
Addiction
Drugs

Ant Pheromone Study May Improve Mental Health Outcomes
Exclusive
Mental Health
Addiction
Drugs
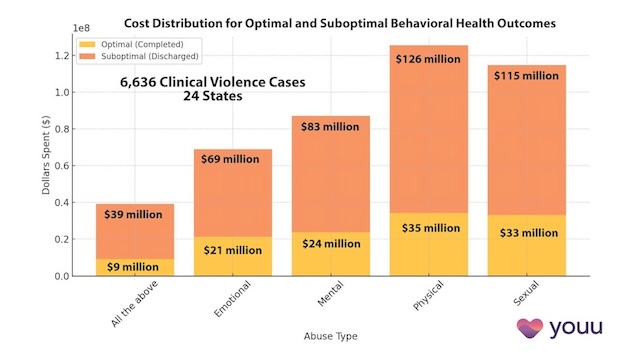
Interrupting Violence Should Be Irresistibly Investable
Exclusive
Mental Health
Addiction
Drugs
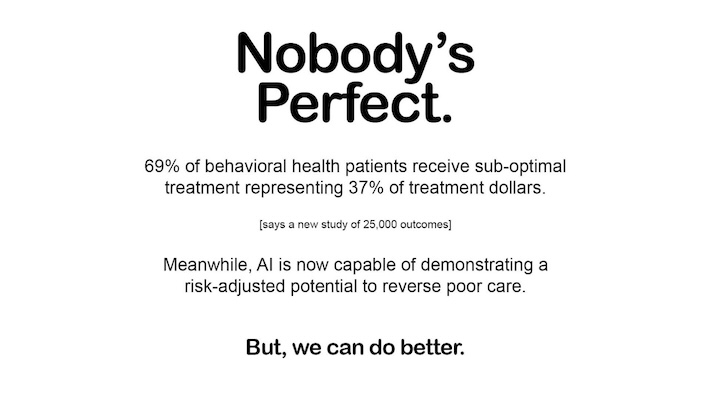
69% of Behavioral Health Patients Receive Sub-Optimal Care According to a New Analysis
Exclusive
Mental Health
Addiction
Drugs
Other Blogs
Have Questions? Lets Meet
Select a time you like to meet with us