Published Date:
Mar 13, 2025
Exclusive
Mental Health
Addiction
Drugs
69% of Behavioral Health Patients Receive Sub-Optimal Care According to a New Analysis
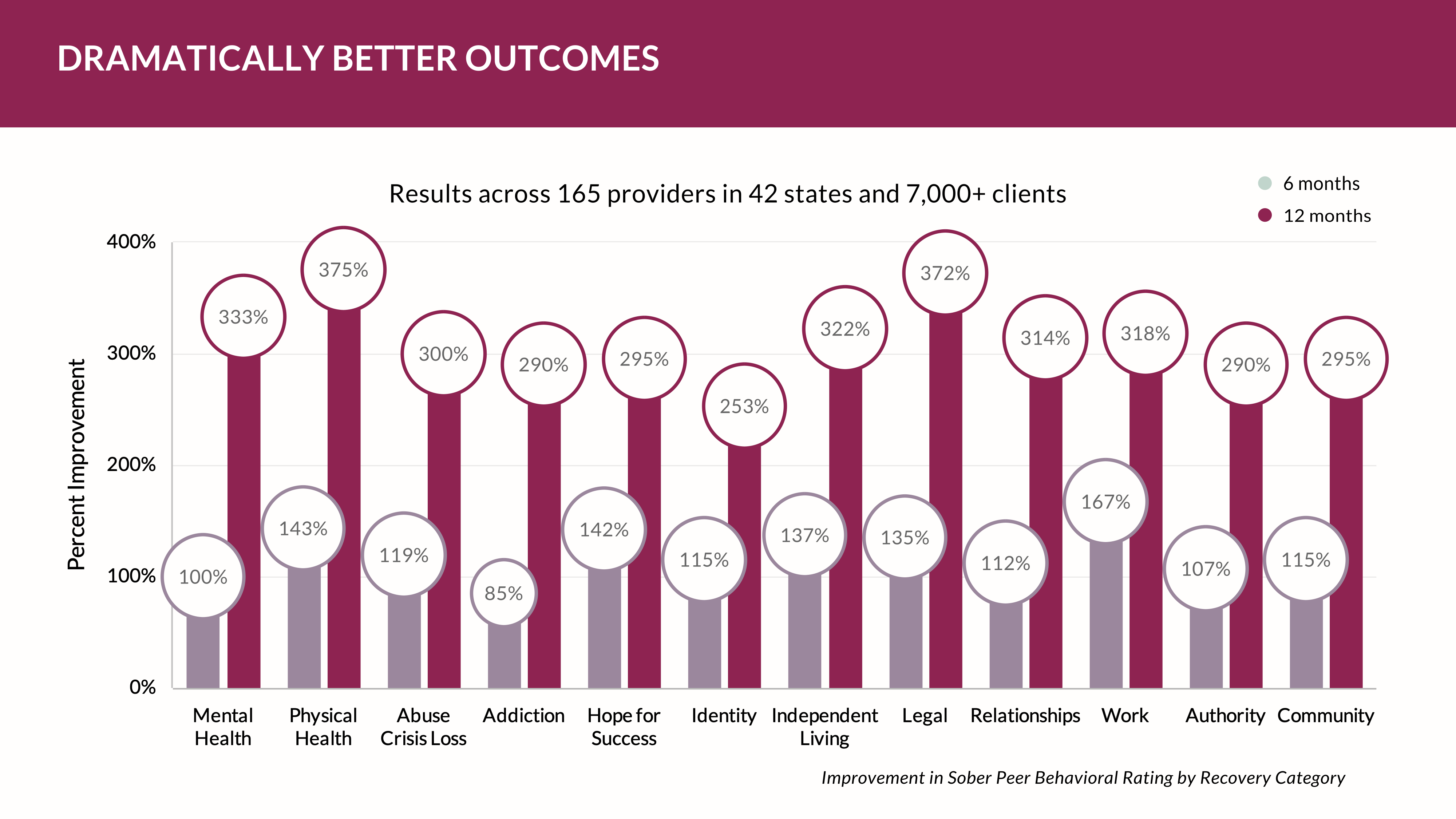
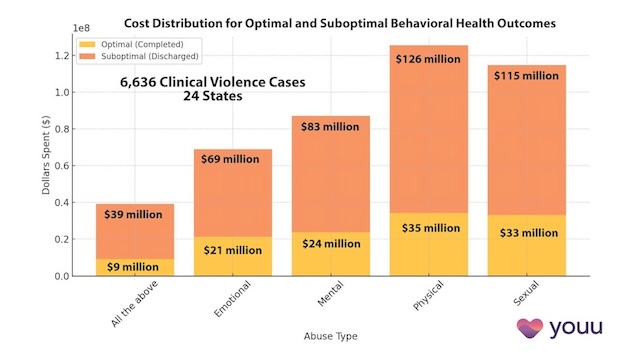
A recent analysis by YOUU Health covering 25,688 behavioral health (BH) treatment cases with expenditures exceeding $740 million, has revealed a startling trend: 69% of patients receive less-than-optimal care. Sub-optimal care definitions were based on provider discharge record determinations.
This finding underscores an indisputable need for systemic changes in how resources are risk adjusted, allocated and how treatments are designed to achieve better outcomes for the majority of patients.
The data tells a compelling story of inefficiencies, highlighting the need for integrated social determinants of health (SDOH) strategies while the potential for artificial intelligence (AI) to learn predictive care delivery economics is now achievable.
Discrepancy Between Dollars and Outcomes
The data analysis reveals an imbalance in the allocation of financial resources and the outcomes achieved -- driven largely by lack of visibility and fee-for-service compensation -- which encourages volume versus value. Of the total $740 million spent on these 25,688 cases, 63% of dollars ($464 million) went towards successful treatments with optimal outcomes, despite serving only 31% of clients. Meanwhile, 37% of dollars ($276 million) were allocated to less optimal treatments, which accounted for 69% of clients.
This discrepancy suggests that while optimal treatments are resource-intensive (costing on average $58,611 per patient on a fully burdened cost analysis), they currently fail to address the needs of a sizable portion of the population. Conversely, most clients receiving less-than-optimal care indicates a gap in either the effectiveness of these treatments or the ability to address underlying factors influencing outcomes – particularly where those risks can be adequately determined by AI machine learning models prior to treatment, and that are not now considered.
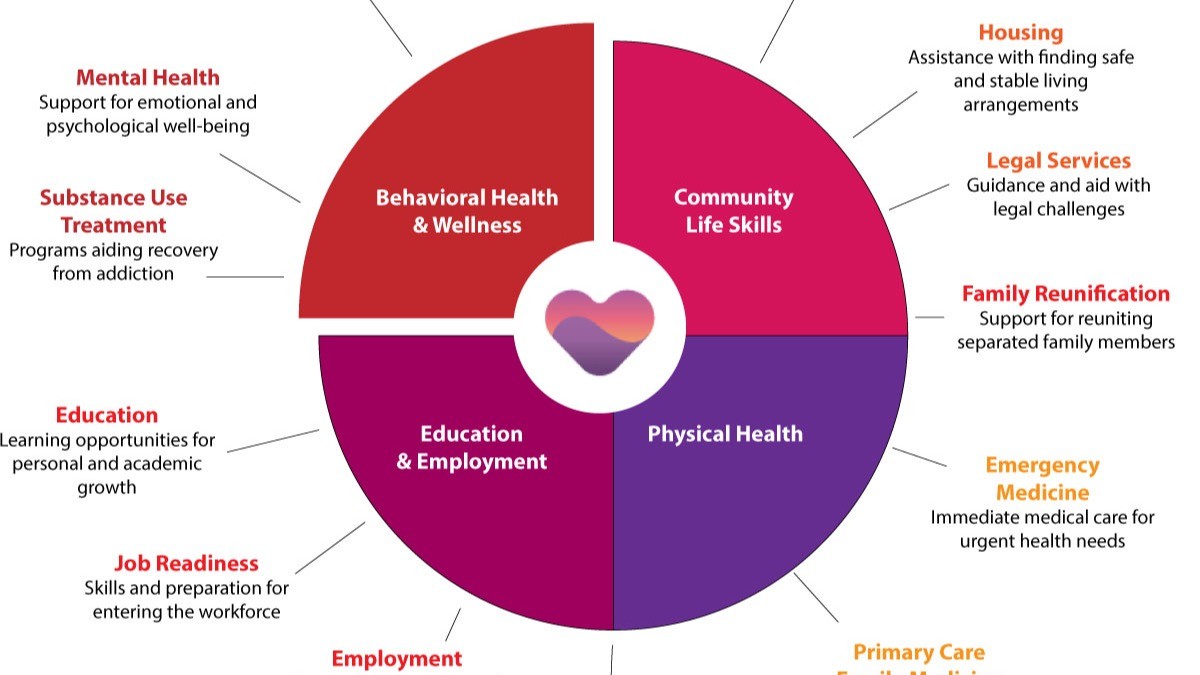
The Epidemical Role of Social Determinants of Health
The analysis further points to the epidemical influence of social determinants of health (SDOH) on treatment outcomes. SDOH factors—such as income, education, health, legal issues, housing, and access to transportation—often determine up to 80% of health outcomes, according to some industry estimates, versus clinical interventions alone. For instance, patients with stable housing and access to nutritious food, or are free of legal complications or violence are more likely to adhere to treatment plans and achieve better results than those facing socioeconomic hardships.
This aligns with the disproportionate allocation of resources: patients receiving successful treatments may benefit from better baseline conditions and additional support systems that enhance their ability to recover.
AI: The Key to Better Predictive Models Signaling Optimal Outcomes
Artificial intelligence could hold the key to bridging this gap by predicting which patients are likely to succeed or struggle with treatment.
Specifically, machine learning algorithms can analyze vast clinical datasets to identify patterns and risk factors associated with treatment outcomes.
By incorporating epidemical data on SDOH, clinical history, and treatment adherence, AI models have proven successful in providing actionable insights to healthcare providers. In most cases, machine learning models need only to access a dozen attributes (out of hundreds collected) to accurately risk-adjust treatment and determine the probable outcome and lifetime cost of treatment, the study suggests.
For example, AI tools help to:
- Identify At-Risk Patients: Highlight patients likely to experience suboptimal outcomes and provide targeted interventions.
- Optimize Resource Allocation: Direct resources towards areas with the highest potential for improvement, such as preventive measures or enhanced support systems for at-risk populations.
- Personalize Care Plans: Provide perspective to tailor clinical treatment plans based on individual patient profiles, increasing the likelihood of success.
Strategies for Improvement
To address these challenges, healthcare systems could adopt a multifaceted approach that combines resource optimization, SDOH integration, and AI-driven insights:
- Reallocate Resources: Increase funding for treatments serving the 69% of patients in the less successful category. Focus on preventive measures and early interventions to reduce the need for intensive treatments later.
- Address Social Determinants: Integrate SDOH assessments into patient care plans. Collaborate and network among community organizations to provide care-assistance for housing, food security, and transportation support.
- Leverage AI: Develop novel predictive models to identify patients at risk of poor outcomes. Use AI insights to tailor interventions and track their effectiveness over time.
- Focus on Cost-Effective Care: Standardize protocols for successful treatments to reduce costs without compromising quality. Experiment with alternative approaches for less successful treatments to identify more effective methods.
A Path Forward
This analysis highlights an urgent need to rethink the allocation of resources and the design of treatment strategies for behavioral health patients.
The 69% of patients receiving suboptimal care represent a critical opportunity for improvement, both in terms of patient outcomes and system-wide reallocation of financial resources ($276 million) previously directed to inefficient or ineffective treatment.
By addressing social determinants of health and leveraging the power of AI, healthcare providers can move towards a more equitable and effective model of care and transition away from perverse fee-for-service incentives.
The road ahead requires collaboration across sectors, innovative thinking, and a commitment to putting patients at the center of care. Can these efforts, the disparity between dollars spent and outcomes achieved be narrowed, creating a system that truly meets the needs of all patients?
We’ll be watching.
Let's Talk. Jump on my calendar to discuss your case for optimal care and AI risk determination.
Subscribe to edTalk for more population health perspectives.
Ed DeShields is Chairman of Community Assurance, a consolidated holding company that includes HealthIT companies including YOUU Health’s platform, the YOUUniverse, that helps communities build their own private, local care networks without the usual barriers that make it hard to understand patient results, risks, access, and cost.
We put the power back in the hands of team care by offering a simple, connected platform that leads to more responsible, member-focused care.
Other Blogs
The Plan No One Sees Coming—But Soon Will
Exclusive
Mental Health
Addiction
Drugs

Ant Pheromone Study May Improve Mental Health Outcomes
Exclusive
Mental Health
Addiction
Drugs
Interrupting Violence Should Be Irresistibly Investable
Exclusive
Mental Health
Addiction
Drugs
69% of Behavioral Health Patients Receive Sub-Optimal Care According to a New Analysis
Exclusive
Mental Health
Addiction
Drugs
Other Blogs
Have Questions? Lets Meet
Select a time you like to meet with us